Last updated on Dec. 3, 2024 at 11:01 a.m.
Erik Nelson, professor in LAS, is pioneering research that could reshape medicinal therapy against cancer. His team’s recent work focuses on the NR0B2 protein, which is found on the surface of nuclei in several different human cell types. It has shown a potential to alter immune cell behavior in ways that may significantly curb tumor growth.
Two papers published in June and August by Nelson and his team in the journal “Cancer Letters” detail their investigation into how NR0B2 can reprogram immune cells within a tumor’s microenvironment to prevent cancer progression and spread. Exploiting this effect could provide hope for patients whose cancer does not respond to standard therapies such as chemotherapy and radiation.
“NR0B2 was originally classified as being very important for regulating cholesterol, especially how the liver handles cholesterol,” Nelson said. “So if you have lots of cholesterol, then your body starts metabolizing that and, ultimately, it turns into bile acids.”
The bile acids produced by the human body as they break down cholesterol serve as a feedback signal. This causes an increase in NR0B2, which serves as an indicator to halt further cholesterol breakdown.
But Nelson and his team discovered a new role for NR0B2, specifically in maintaining a balance of T cells, a type of white blood cell that helps humans fight infection and disease.
Get The Daily Illini in your inbox!
When NR0B2 is activated in myeloid immune cells, one of the human body’s first lines of defense against illness and infection, the myeloid immune cells talk to T cells. It directs them to either develop into one of two types: effector T cells or regulatory T cells.
Regulatory T cells — also known as Treg cells — normally have an important function as the brakes on the immune system, according to Nelson. But in cancer, Tregs favor the growth and spread of tumors. Too many Treg cells lead to poor prognoses and responses to current therapies.
The team is also studying a small compound, DSHN, and a derivative of that compound, DSHN-OMe. These both activate and increase the activity of NR0B2. NR0B2 can then influence the myeloid immune cells. This leads to a decrease in regulatory T cells and a greater immune response against the tumor.
“We worked with chemists here, led by Paul Hergenrother in chemistry, and they developed a series of derivatives of DSHN using their medicinal chemistry as a background,” Nelson said. “We took those derivatives and tested them in our lab for better properties, and especially their ability to inhibit these regulatory T cells.”
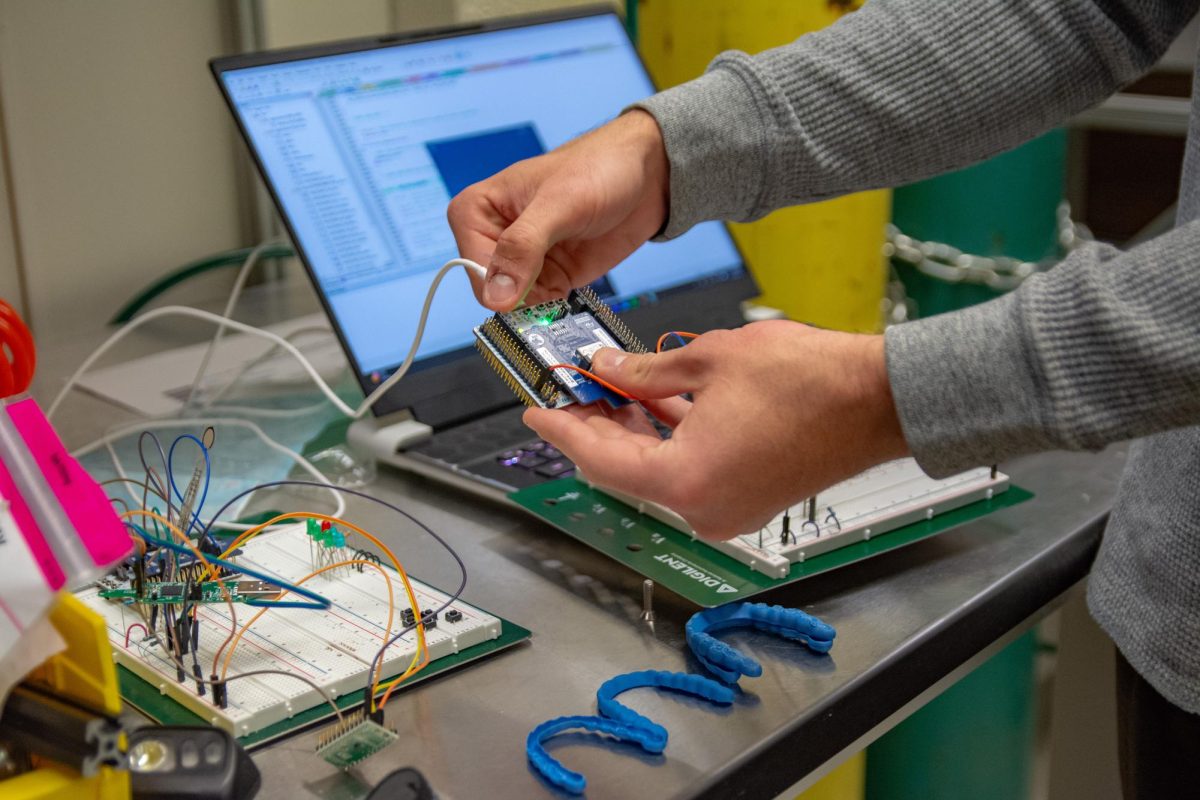
Nelson and his team also screened the DHSN derivatives for toxicity and concluded that DHSN-OMe was the most effective at decreasing levels of Tregs.
“If we’re thinking about getting a drug into humans, we wanted to have low toxicity,” Nelson said. “Ultimately, we came up with a winner, if you will, and that was DHSN-OMe.”
Nelson explained how DHSN-OMe has demonstrated anti-cancer effects in preclinical models of breast cancer, including human cell cultures. Now, the team wants to transition their laboratory findings to medicinal treatments, a process known as translation.
“First, we need to better understand (the molecule’s) pharmacokinetics,” Nelson said. “When we put the drug into an animal, where does it go and how does the animal handle that? And so we’re starting with mice, and ultimately, we’ll move it into higher vertebrates.”
Nelson said a goal of the project is to enlist the help of the University’s College of Veterinary Medicine for conducting clinical trials in pets and using those results as a stepping stone to transitioning the medication to humans.
Nelson’s research is supported by the Beckman Institute for Advanced Science and Technology, the Cancer Center at Illinois and the Carl R. Woese Institute for Genomic Biology. His research has additional support from interdisciplinary collaborations that strengthen their studies’ rigor and applicability.
“I am an expert on a certain number of things,” Nelson said. “But in order to move this ultimately into humans, I need expertise in several different areas to help push that.”
Nelson said one of the key motivators for his team’s research comes from the stories shared by cancer survivors and advocates who have experienced the limitations of current therapies.
“We work very closely with a group called the cancer research advocacy group,” Nelson said. “It’s a collective of survivors, people with ongoing treatment for cancer, caregivers, clinicians and researchers.”
The group helped Nelson and his team identify gaps in clinical care, especially in areas like postclinical support and survivorship issues. By understanding and acknowledging these shortcomings, Nelson hopes to tailor his lab’s research toward practical applications that could improve patients’ quality of life.
“That is really motivating for us — hearing their stories and them saying where the shortcomings in clinical care are,” Nelson said. “It’s very inspiring … I think we’re all touched by someone we know that has been diagnosed with cancer and had to live through that, or potentially, we’ve lost close people to it.”
Nelson has found moments of immense reward in his career, particularly when a research project succeeds after years of rigorous trials and testing. He has previously helped develop an anti-cancer therapeutic drug that received FDA approval for human use.
“I was really fortunate to be part of an idea while I was a postdoctoral associate at Duke University, where I helped position a drug for the treatment of metastatic breast cancer,” Nelson said. “Now, that drug is FDA approved and actively prolonging people’s lives.”
However, he acknowledged that the journey from lab discovery to clinical application is rarely straightforward. Securing funding for innovation remains a struggle, even when the potential for impact is significant. Nelson also offered guidance for aspiring scientists, describing the variety of research paths available. He said young researchers should carefully consider their career goals and the unique contributions they want to make in academia, industry or government.
“There are different ways to pursue research,” Nelson said. “You have to decide where you want to go with your career and what style of research you want to do, such as in an academic setting, in an industry or pharmaceutical setting or the government setting.”
That’s not the only way to contribute to scientific innovation, though. Nelson said young scientists can also set up foundations that help manage research and lobby the government to change legislation.
“Do your homework and find the areas that suit you the best,” Nelson said.
For Nelson and his team, the ultimate goal is to translate his lab’s discoveries into tangible improvements in cancer treatment. By advancing new therapies that harness the body’s own immune system, he said he hopes to provide better options for patients fighting cancer.