UI professor works to rebuild bones
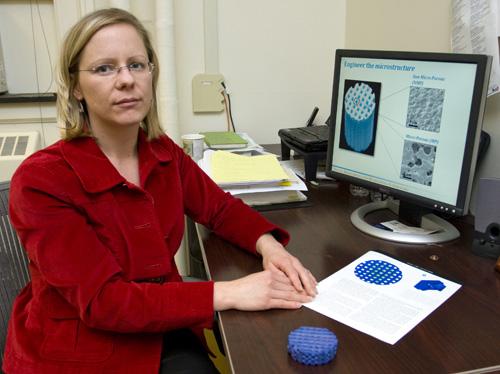
Professor Amy Wagoner Johnson displays diagrams and a scale model of a synthetic bone implant she developed. The implant is only a few millimeters in diameter and replaces the scaffold in a bone, which helps it regrow. Erica Magda
December 11, 2008
The few days of living on a liquid diet after having wisdom teeth removed can be annoying, but imagine living that way for more than a decade after losing part of a jaw bone to cancer.
University professor Amy Wagoner Johnson is researching and testing different methods of rebuilding bones to help restore function and appearance.

“There are a lot of cases where people have large bone defects or load-bearing bone defects, and there is no good solution right now,” said Wagoner Johnson, a mechanical engineering professor. “Metal implants are too stiff, and the bone disappears around it.”
Other implant procedures, such as harvesting bone from the patient’s hip or from a cadaver, can cause complications and infections, Wagoner Johnson said.
Get The Daily Illini in your inbox!
“We’re trying to develop a synthetic material, called a scaffold, that bone can grow into,” she said. “In the future, we could use a CT scan to get the shape of a patient’s defect and do simulations to find the right support.”
The synthetic scaffold is made from hydroxyapatite, a calcium phosphate mineral very similar to the mineral part of bones, she said.
Wagoner Johnson and her research team are using micro computers to aid in the building of scaffold models.
“We basically took a CT scan of a scaffold with a micro computer and characterized how bone was growing in these scaffolds,” she said. “From that information and previous studies, we made a simple model, called a unit cell model.”
With the model, Wagoner Johnson’s team is looking at tuning the structure and pore size of the scaffolds as well as looking at how any structural changes affect mechanical properties.
“We’ve had lots of evidence that shows that by adding pores to these scaffolds, you can really improve bone growth,” she said. “We’re really trying to understand why that happens, so we can exploit it more.”
Wagoner Johnson works alongside graduate students and other professors to make the research more time and cost efficient.
Graduate student Sheeny Lan is researching blood vessel formation to encourage bone growth.
“My approach is to use adult stem cells that can differentiate into cells that form blood vessels and incorporating them into the scaffold,” Lan said. “The major barrier is that you need blood vessels to be there for tissue to regenerate.”
Sam Polak, a graduate student, studies the structure of the synthetic scaffolds.
“I’m looking at the mechanics of the scaffolds and how any structural changes can affect it,” Polak said.
In the future, the structure and shape of the bone scaffold material could be tailored to each patient’s need, Wagoner Johnson said.
“The synthetic bone scaffolds could be used on a smaller scale in possibly five years,” Wagoner Johnson said. “However, use for really massive defects is a ways off because you have to go through steps with the FDA to get it approved.”
Anthropology a ssistant professor John Polk, who focuses on biological anthropology said the bone scaffold has the potential to be used for many different situations.
“I know the research team had been thinking of working with people with mandibular, or jaw, defects, but this could also be used for bone tumors, severe breaks and other things,” Polk said.
“Once it is successful for human use, it could be very important for veterans who have had various combat injuries.”






